Palliative Care At Home
Palliative care is an approach that improves the quality of life of patients and their families facing the health issues associated with a life-threatening illness, through the prevention and relief of symptoms and suffering by means of early identification, assessment, treatment of pain and other problems, physical, psychosocial and spiritual – World Health Organisation.
In Home Palliative Care is one of our very special services.
Did you know 82% of Australians think it’s important to talk to their family about how they want to be cared for at the end of their lives? But only 28% have. [4]
Did you know 70% of Australians would prefer to die at home…yet only 14% do? Unfortunately, 54% die in hospital and 32% die in a nursing home (1) – their least preferred places to die.
Did you know Australia’s rate of deaths at home is comparatively low compared to our peers? In fact less than half the number of Australians die at home compared to people living in New Zealand, the United States, Ireland and France.(1)

It is surprising that so few elderly people get their wish to die at home when two thirds of Australians die between the ages of 75 and 95. (2) Their deaths are more predictable and we have longer to plan as we survive acute illnesses, accidents and live many years with chronic diseases such as heart disease, diabetes, dementia, Parkinson’s etc.
Today about 70% of deaths are expected and therefore could have been spoken about and planned for. We believe that’s because clients and their families don’t understand, in advance, what dying at home entails.
We’d like to help more Australians fulfil their wish to die at home and to pass over peacefully, pain free and surrounded by the love of their family and friends, in the comfort and familiarity of their home.
Over 82% of Daughterly Care’s caring role is providing:
- Care to clients with high care needs (assessed by the Aged Care Assessment Team (ACAT) as high-care levels 3 and 4);
- Palliative care; and
- End of Life care for our clients.
In our 27 years, all our In Home Palliative Care clients, have died peacefully and pain free, surrounded by loving family, friends or us at home, in line with their wishes.
During the Palliative Care and end of life care stages our Registered Nurses and experienced Caregivers are taking medical direction from:
- The client
- The Community Palliative Care Doctor
- The Community Palliative Care Registered Nurses
- The client’s GP
- The client’s family / Enduring Guardian
Daughterly Care is engaged in different ways to assist during the palliative and end of life care stages depending on the needs of the client and client’s family.
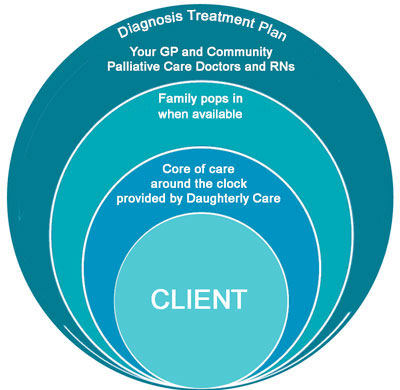
During most of the End of Life care we provide, Daughterly Care’s highly experienced Live in Carers and Registered Nurses provide the core of the nursing care full time. Our Live In Caregiver or 24 Hour Caregivers and our Registered Nurses step back to give privacy when family are present.
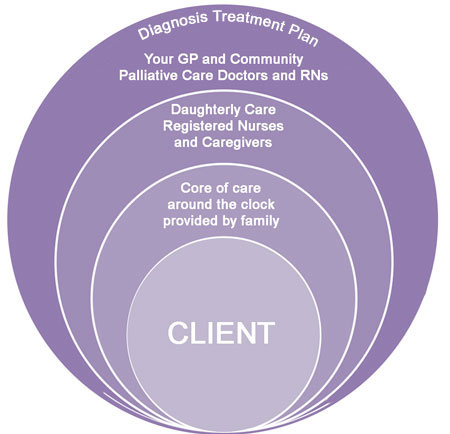
Alternatively family is providing the core of care and our Caregivers or Private Nurses are bought in at specific times, such as overnight, to give family a proper deep sleep so they can carry on caring the next day.
When the free Community Palliative Care Registered Nurses are not available our Private Registered Nurses are engaged to administer medication that controls pain and eases anxiety, as well as provide care.
When the decision is made to have End of Life care at home, we can provide advice on what is needed to professionally and comfortably care for your Loved One or yourself.
The Government funds 48 hours of End of Life care when it has been approved by the Community Palliative Care Team. This care can be contracted to Daughterly Care so that you can continue to have your known and trusted Live in Carer or Hourly Caregivers providing the care.
Continuity of care with known and trusted Caregivers is really important and makes the end of life journey easier as they are familiar with the Elder and his/her condition, family, home and know how you like care delivered.
Your GP or the Hospital Doctor must refer you to the Community Palliative Care Team. It takes time for the Registered Doctor and RN to come to your home and register you with the service. At that initial meeting they find out about you and your condition. Just because you are registered doesn’t meant they start treatment. They only do that when treatment is needed.
- Your GP or hospital Doctor will refer you to the Community Palliative Care Team
- The Community Palliative Doctor and Registered Nurse visits your home to meet you and find out how you are coping with your condition/illness. With your permission, they register you with their service. It typically takes 1 to 2 weeks for the Registration visit to occur. This is why you don’t want to leave Registration until the last days. Typically our Live in Caregiver and/or High Care Case Manager or Registered Nurse will attend this meeting.
- No treatment starts until you need Palliative or End of Life Care. You remain in control.
- When the time comes that you need their specialist assistance you, your family or Daughterly Care calls the Community Palliative Care Team and asks for them to attend. Typically they attend the day after we call.
- Pallation starts. They start small and only give what you need to feel comfortable.
- The Community Palliative Care Registered Nurse follows the treatment plan decided by the Community Palliative Care Doctor. Typically they train the family how to administer the “break-through pain relief.” So if the current medication stops relieving all pain, they explain how to increase the pain relief. Legally paid Caregivers cannot administer the break-through medication. If family are not able to administer break-through pain relief, Daughterly Care’s Registered Nurse can.
For 27 years Daughterly Care’s experienced and professional Caregivers have provided the Palliative and End of Life care for our Live In Care clients, so we have vast experience in this specialised field.
Palliative Care is a journey that is so much more than satisfying the nursing needs of the client. It’s about caring for the mind, spirit and body of the client. It’s also about supporting the Elder’s family. Our role is to be sensitive and supportive to the client and the family in a way that is emotionally intelligent and practically helpful. We know it is a very sensitive time, full of emotion and therefore an extremely tiring time for family, even when they are not providing the ‘hands on’ care.
“It’s a big effort, given willingly, from a place of great love and respect …and a journey that families always say they were pleased they gave to their partner, parent or friend.”
And frankly, it’s a journey that is made much easier with our experienced Live in Carers and Registered Nurses guiding you and advising you each step of the way.
21 October 2016 – Appreciative Email from Daughter of Palliative Live in Care Client from Gerringong, on South Coast of NSW
Dear Penny and the team,
Many thanks for the wonderful support you’ve given to both myself and Dad over the past few months. It’s been such a comfort to have a truly committed and caring team assist in all aspects of Dad’s care.
Thank you for your wisdom and gentle guidance along the way, and above all for just being there and allowing Dad to live out his days as he truly wished, in the comfort of his own home in beautiful Gerringong.
Best wishes,
Lindsay
How does Palliative Care in your home work?
Typically when our client reaches the Palliative Care stage, our High Care Manager will recommend you ask your GP to make a referral to the Community Palliative Care Team to arrange for their invaluable palliative care and end of life care services. They are specialists in this area. It is their calling – day in, day out.
The Community Palliative Doctor’s role is to diagnose and determine a Treatment Plan to best manage the symptoms of the illness or condition, including pain management and prescribes the appropriate medication(s).
The Community Palliative Care Registered Nurse follows the Treatment Plan set by the Community Palliative Doctor and provides any medications needed. Once upon a time Community Palliative Registered Nurses would visit to administer all medication as needed each day…but now there are so many people they need to visit, so instead they train up family on what needs to be done in between their visits. If the family doesn’t feel confident administering medication such as morphine then our Registered Nurses will.
They only increase the medication if and when you need that.
No Regrets
Tip: Make sure that all family members and significant others have said their final goodbyes BEFORE any morphine is administered because by this stage the person can quickly become unconscious.
In our experience, our clients will typically pass away within 1-3 days of receiving morphine via a butterfly needle in their thigh attached to a morphine pump.
Organisational Tip:
It is very important that a “Known Doctor” can attend the home to sign the Death Certificate within 8 hours of the death. So keep in daily contact with your GP. If your GP is going on holidays then immediately organise for the Locum Doctor to attend so that she/he becomes a “Known Doctor” and can sign the Doctor’s Certificate. If you do not do this and a Known Treating Doctor cannot attend within 8 hours, then the Police will take the body to the Coroner for an autopsy.
Call the Undertaker, who is conducting the funeral to remove the body.
After the Doctor has signed the Death Certificate, you can wash and dress the body. Washing, dressing, singing and talking to your Loved One can help family members pay their respects and process.
Tip: It’s very important to place the legs straight and the arms straight. Do not cross the arms over the chest as they may need to be broken later. Shut the eyes and wrap a piece of material under the chin and over the head to keep the mouth shut.
Daughterly Care’s role varies tremendously from client to client based on our client’s care needs and their family’s support:
Low key role – when the family is providing most of the care, they use us as a break. They book our services for a block during the day or active night care. This ensures a proper sleep or break for the family members, so they are fresh to provide the care the following day.
Whether we recommend a Registered Nurse or a very experienced Caregiver depends on factors such as:
- Where the client is on their Palliative Care or End of Life journey
- How well we already know the client and what support we already have in place
- The current care needs of the client
- How involved the family is in delivering care; and
- Whether Schedule 8 medication needs to be given as this automatically means a Registered Nurse is legally required to administer the medication, unless the family administers this level of medication
Live In Care – when the client is our Live In Care client – our Live In Caregiver, who may have cared for the client for a number of years, normally provides the core of the Palliative and End of Life care. Depending on the care needs of the client and the care role of the family, rather than move to 24 Hour care where 3 shifts of Caregivers or Registered Nurses are required per 24 hours for care and consistency, we prefer to let our Live In Caregiver provide care during the day and we bring in additional help as and when needed for parts of the day or overnight. Our approach provides the greatest consistency of known and trusted Caregivers at home. Our Registered Nurse attends to administer medication when the Palliative Care Registered Nurse or family cannot.
We are a Safe Pair of Caring Hands
The Client, their family, the General Practitioner (GP), Palliative Care Doctor, Registered Nurses and our staff, all work together as a cohesive team to enable the client to have a “good death”.
What makes a good death? In our experience it is:
-
- Passing over peacefully and without pain;
- To have had control over where you die and how you are cared for;
- To have had the opportunity to have deep connection with those you love by expressing love to them;
- To have had the opportunity to say goodbye to people who are important to you;
- To have had the opportunity to resolve, through forgiveness, outstanding issues with family or friends;
- For the journey to be as stress free as possible for all who are privileged to walk this journey with the client; and

3 Palliative Care and End of Life Client Examples
Example 1
A Northern Beaches Community Palliative Care Registered Nurse said to our Caregiver “In my 21 years of providing Community Palliative Care, this is the most perfect way to die that I have ever seen”.
What had she seen?
Background: A much loved Mother was bought home from hospital to die. One of her children was a Specialist Palliative Care Doctor working in one of Sydney’s leading Hospitals. There were also Registered Nurses in the family. As they were all working full time they engaged Daughterly Care to provide Live In Care. When the client first came home from hospital we assessed that an Experienced Professional Caregiver, rather than a Registered Nurse, would be perfect for the role. Whilst the client was in the palliative care stage she lived 9 months in comfort at home before her end-of-life journey began. During that time she was cared for by two of our experienced Live In Caregivers
During the End of Life care, our Live In Caregivers provided the core of care in between regular family visits. The Community Palliative Care team was brought on the team and we were working under the direction of the family and the Community Palliative Care Doctor or Community Palliative Care Nurse.
Our Live In Caregiver, who had known the client for 9 months, noticed the client was in pain and reported that to the child who is a Specialist Palliative Care Doctor. It was felt that the current pain medication was sufficient. Our Caregiver knew the client’s body language and could see that she was in pain and when she did a “number 2” she searched through it and found the pain medication whole and unabsorbed by the body. So she took a photo to show her child. “Your Mum is in pain and I believe this particular pain relief is not being absorbed by her body…I have seen this before with this particular medication”. Our client was put on a different, more effective pain medication.
Towards the end, our staff moved their bed beside the elderly client’s bed because that’s what the client wanted, and when the family weren’t laying there…we were.
This client had a peaceful, pain free passing at home, surrounded by her loving family.
Example 2
Background: Our Live In Care client had fronto lobe dementia and was aphasic and therefore unable to speak… however she understood every word we said and would answer with foot or hand tapping, eye blinking and head movements.
During the End of Life Care
Her Mosman GP was overheard saying to her Daughter “There is something very special happening in this home. Your Mother is not in any pain and she could not be in better care than with Daughterly Care”.
This client had a peaceful, pain free passing at home, surrounded by her loving family.

Example 3
A niece called us to organise care for her Aunty who she had promised could die at home. The General Practitioner (GP) of the client visited and “said she had to go to hospital because there are Registered Nurses there and she will need Morphine”.
The niece asked us, ‘why is that necessary when Aunty is not in pain?’ We explained that Daughterly Care has Registered Nurses to administer Morphine if the Doctor’s care plan prescribed it. We also explained that all equipment needed, such as an electric lift bed with an airflow mattress could be hired and delivered the same day – which it was.
During the End of Life care
We asked our client which was her favourite room of the house and she said her Sunroom, where she could overlook her garden and tennis court. Our client had not had children and she had fond memories of the neighbourhood children playing tennis in her yard.
Our client “let go” the following day, pain free, no morphine needed.
Her niece was so relieved and happy that she had been able to give her Aunty her final wish – to die peacefully and with diginity at home and that her last weeks had been joyful living in her home and her passing over was peaceful and pain free.
If you or a Loved One’s wish to die at home, call Daughterly Care to join your care team – we are a safe pair of caring and experienced hands and will guide you through this journey.
Our live in care client, Mr W died on Saturday 17th. Mr W’s wife rang to thank her Live in Carer angels, Nichole S and Karen S. Mrs W said that she didn’t know what she would have done without Nichole and Karen. She was pleased she had managed to keep her promise to her husband and bring him home for a few days. This made his death a little easier. Mrs W said that she fell into a hole a few times and both Nicole and Karen were there to catch her and she couldn’t be more thankful. Her daughters were also very grateful that they knew their mother had two exceptional carers there to help her. Both Nichole and Karen said it was a pleasure being with this family, there was something very special about them.
Jean, High Care Case Manager
Dear Daughterly Care Community Services, I wanted to drop a note to thank you and your team on behalf of my Mum and Dad, and our family. The last 5 months have been very difficult for our family and your team have done a fantastic job – both in terms of the support provided to Mum and Dad, and also the calm and efficient manner in which this support has been provided.
I also wanted to call out a few of the carers for their exceptional work – Annie, Lute and Marnie. These lovely women have been instrumental in helping us navigate the last couple of months, demonstrating compassion and patience for our parents as well as our family.
I have been so impressed with the care that I have observed being given to [name withheld] of Rose Bay that I have decided to bring my husband home from hospital with Daughterly Care on board tomorrow. I think Daughterly Care is wonderful.
| 6 November 2015 – Words of appreciation from the son of a client in Hunter’s Hill
Hi All, Just wanted to share with you a comment from the son of a Palliative Care [Live in Care] client who has just passed away with our Caregiver Margaret M caring for the client. Margaret said the gentleman had asked for eggs and toast for tea, which he ate by himself. He said he was in no pain. The family had all been to visit and had said their good-byes for the day. The gentleman had been conversing with Margaret and was in good spirits. Margaret had just finished changing his pad and went out of the room for a few moments when the co-resident son came in and asked if Dad had been making breathing noises and Margaret replied “No” when they walked back into the room to find the client had passed away. After Margaret had hugged all the family and finished her duties, another son, James, said he would carry her bags out to her car. On the way to the car, James told Margaret that he was extremely impressed with Daughterly Care’s services and thanked her for all she had done for his father and their family. |
 Click here to view Margaret’s profile Click here to view Margaret’s profile |
| “When I went into Mum’s room, the day before she died, Fairy [Daughterly Care Caregiver] was sitting quietly, gently massaging lanolin into Mum’s arms and hands. Mum looked so peaceful and relaxed and was obviously enjoying every minute of it! Fairy was a Godsend at a time when I was feeling a bit lost and alone. Fairy knew how to connect with Mum; no words were necessary.” |  |
| Click here to view Fairy’s profile |
Read unsolicited feedback from our clients. We’re always thrilled to receive such kind words.
The next step is easy … contact us for a confidential chat about your needs or to organise your, free no obligation consultation email claireg@daughterlycare.com.au or call us on (02) 9970 7333.
1. Swerissen, H & Duckett, S, September 2014, Dying Well, Grattan Institute, Report No 2014-10, September 2014 p.4
2. Australian Bureau of Statistics (2013b) Deaths in Australia, 2012, 33020DO019, Australian Bureau of Statistics
3. Swerissen, H & Duckett, S, September 2014, Dying Well, Grattan Institute, Report No 2014-10, September 2014 p.5
4. www.dyingtoknowday.org

